An estimated 1.9 million people, around 3% of the UK population, have long Covid and of those, nearly three-quarters are experiencing disabling symptoms of fatigue.
Fatigue can hugely impact your quality of life. Here at Newcastle University, we want to understand the pathology of SARS-CoV-2. Dr Mark Baker, Senior Clinical Lecturer at Newcastle University, discusses a recent breakthrough that could help medics treat symptoms for long Covid sufferers.
I have been caring for patients as a neurologist in the NHS for over 20 years and one of the most challenging symptoms to manage in any chronic neurological disease is fatigue. Whilst fatigue may be common in chronic neurological diseases such as stroke, multiple sclerosis (MS) and motor neurone disease (MND), affecting 80-90% of patients, it is very difficult to treat and therapeutic options are limited.
Covid-19 and post-viral symptoms
Global crises have a habit of generating rapid scientific advancements. The SARS-CoV-2 pandemic is no exception. Whilst there have been very high-profile developments, the most notable of which has been the revolution in vaccine development, Covid-19 has also provided the scientific community with the first opportunity in over a century to study large numbers of people experiencing persistent post-viral symptoms. The large numbers mean that we can detect small but significant correlations and have greater statistical certainty about results.
After a viral infection it is rare for symptoms to persist beyond 12 weeks. However, according to the most recent data from the UK Office for National Statistics ONS, approximately 2.9% of the population are reporting persistent symptoms after Covid 19, nearly three-quarters of whom are experiencing disabling symptoms of fatigue, known as post-Covid fatigue (pCF).
Post-Covid fatigue and our research
We have seized this opportunity and, led by my colleague Dr Demetris Soteropoulos, with funding from the Medical Research Council (MRC), carried out behavioural and neurophysiological tests on people suffering from post-Covid fatigue and compared them to people without fatigue.
In 37 people with pCF and 52 age-matched controls, we tested 35 physiological and behavioural indices that measure function in the:
- brain
- spinal cord
- peripheral nervous system
- muscle
- autonomic nervous system
Our breakthrough findings
Our results, now published in Brain Communications, show that 10 of these measures were significantly different from controls without fatigue, encompassing three specific areas of the nervous system:
- A slower reaction in specific areas of the brain because of underactivity in specific cortical circuits.
- An imbalance in the autonomic nervous system – the network of nerves that regulates unconscious body processes such as blood pressure and the rate of breathing was found to be impaired. This can have wide-ranging effects on several different body processes.
- Muscle abnormalities - muscle fibres became more easily fatigued after exercise than in people without post-Covid fatigue.
What was striking was that the changes in the autonomic nervous system in those with pCF looked like what you might expect to see if the vagus nerve were underactive.
What is the vagus nerve?
The vagus nerve has been described as the ‘hidden housekeeper’ of the body. By connecting the brainstem to organs such as the heart, lungs, spleen and gut, it can control important automatic functions of the body such as heart rate, blood pressure, inflammation and digestion.
At the same time, Professor Fai Ng and colleagues at Newcastle University, who have for many years been investigating fatigue in Sjögren’s Syndrome (a chronic immune-mediated rheumatological condition), had shown similar autonomic changes in their patient group as those we observed in pCF.
Moreover, studies completed before the pandemic also showed that non-invasive vagus nerve stimulation can improve symptoms of fatigue in this patient group.
The similarity of these findings led us to hypothesize that vagus nerve stimulation could improve symptoms of fatigue in patients with pCF.
Current trials and future research – non-invasive vagus nerve stimulation
With funding from the National Institute for Health Research (NIHR), we are currently trialling a non-invasive method of stimulating the vagus nerve.
This involves clipping an earpiece to the tragus on the ear and delivering small electrical currents using a transcutaneous electrical nerve stimulation (TENS) machine – familiar to many through its use for pain relief during childbirth.
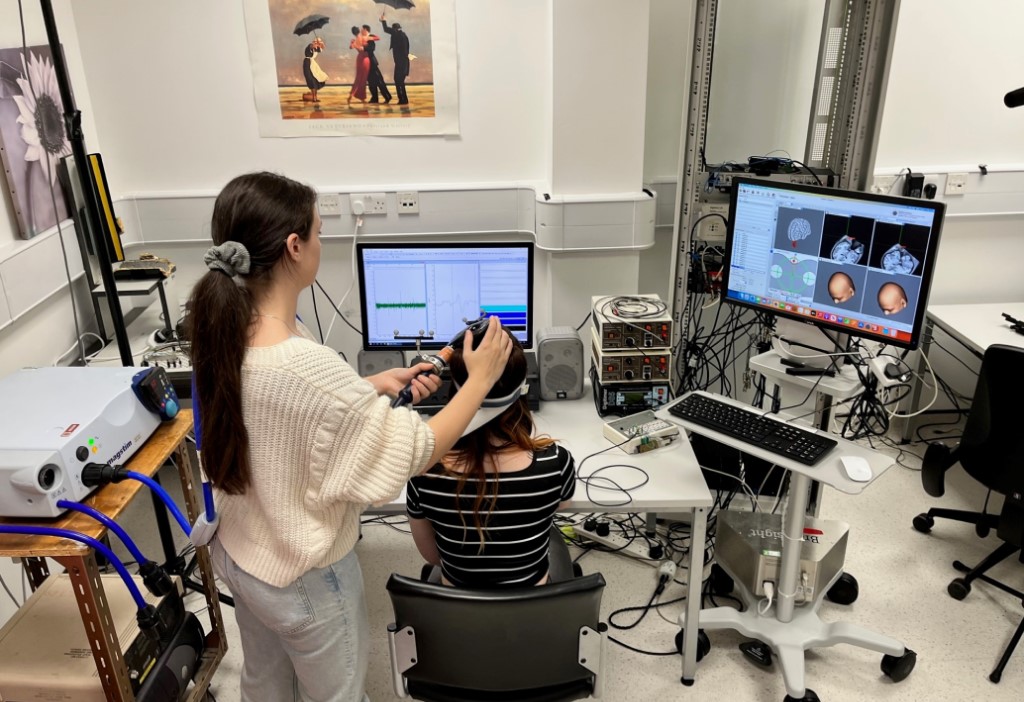
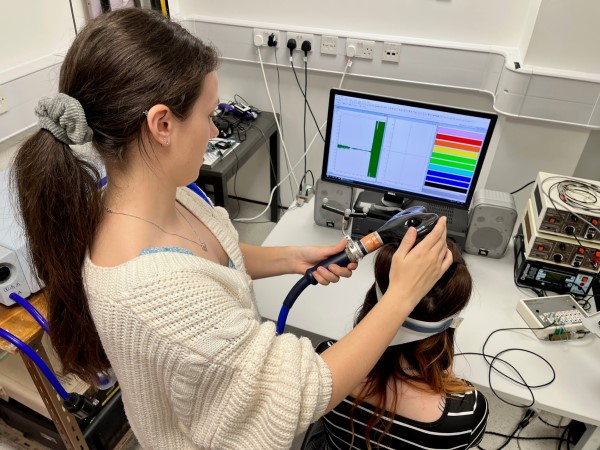 Nathalie Maffitt, Research Assistant and paper co-author carrying out Transcranial Magnetic Stimulation on patient Robyn Newby
Nathalie Maffitt, Research Assistant and paper co-author carrying out Transcranial Magnetic Stimulation on patient Robyn Newby
This project aims to:
- Establish whether vagus nerve dysfunction is important mechanistically in post-COVID fatigue.
- Test whether boosting vagus nerve activity with TENS can improve symptoms of fatigue.
- Identify neurophysiological and immunological biomarkers.
Implanted Vagus Nerve Simulation (VNS) has been used to treat epilepsy for decades, but with the arrival of non-invasive devices, vagus nerve stimulation is promising for treating other disorders. Dr Alison Yarnell, also at Newcastle University, is currently running a trial of non-invasive VNS in Parkinson's Disease.
Covid and its aftermath will always be part of our world. And for this reason, we need to continue to be at the forefront of its pathology and treatments.
You might also be interested in
- Neural Dysregulation in Post-COVID Fatigue. Anne M.E. Baker, Natalie J. Maffitt, Alessandro Del Vecchio, Katherine M. McKeating, Mark R. Baker, Stuart N. Baker and Demetris S. Soteropoulos. Brain Communications.
- Our recent news story about Dr Baker and Dr Soteropoulos's research
- The Covid fatigue trial website
- Autonomic Nervous System Dysfunction in Primary Sjögren’s Syndrome. Davies K, Ng W-F. Frontiers in Immunology 2021, 12, 702505.
