How is our new method for scans transforming lung research?
27 May 2025 | By: Newcastle University | 3 min read
Respiratory disease is the third largest cause of death in the UK. Now, a revolutionary new method of scanning lungs could help medics identify any decline in lung function sooner.
Led by researchers here at Newcastle University, this new scan method uses a gas called perfluoropropane, which can be imaged with advanced MRI (Magnetic Resonance Imaging) scans to show the effects of treatment on lung function in real time. It can also provide insights into how transplanted lungs are functioning.
Read on to discover how this research will have ground-breaking implications for patient outcomes and the clinical development of new treatments.
Contents:
- Lung disease in the UK
- What does the new scan method do?
- Use in lung transplants
- Better outcomes for patients
Lung disease in the UK
Respiratory disease affects one in five people and is the third biggest cause of death in England, after cancer and cardiovascular disease.
Lung disease refers to a broad range of disorders that impair the normal function of the lungs, and impact breathing and overall health. These conditions can affect the airways, the lung tissue itself, or the circulation within the lungs. The most common lung diseases in the UK include asthma, chronic obstructive pulmonary disease (COPD), pneumonia, lung cancer, and various infections.
Lung disease can be caused by a variety of reasons, including cigarette smoking, infections, environmental exposures, and genetic factors. Smoking is a primary cause of many lung diseases, while infections from bacteria, viruses, or fungi can also lead to conditions like pneumonia. Environmental factors like air pollution, asbestos, and other hazardous materials can also contribute to lung damage.
Since 2018, hospital admissions for lung disease have risen at three times the rate of all total admissions. Incidence and mortality rates from respiratory disease are higher in disadvantaged groups and areas of social deprivation, and the gap is ever widening.
What does the new scan method do?
The new scan method developed by the research team, led by Professor Peter Thelwall, Professor of Magnetic Resonance Physics and Director of the Centre for In Vivo Imaging at Newcastle University, enables the team to see how air moves in and out of the lungs in real-time.
The method uses a gas called perfluoropropane, which is visible on an MRI scanner. This odourless, colourless, non-toxic, and non-flammable gas is safe for patients to inhale and exhale.
After the gas is inhaled, MRI scans track how it moves and where it reaches in the lungs. This allows the team to identify areas where air doesn’t reach as well, which is common in patients with lung disease. By measuring how much of the lung is well-ventilated and how much is poorly ventilated, the team can clearly locate and visualise the lung regions with ventilation defects.
'Our scans show where there is patchy ventilation in patients with lung disease, and show us which parts of the lung improve with treatment. For example, when we scan a patient as they use their asthma medication, we can see how much of their lungs and which parts of their lung are better able to move air in and out with each breath.'
Professor Pete Thelwall
Using these results, it’s possible to make a thorough assessment of a patient’s respiratory disease, and how well it’s responding to treatments, including the widely used inhaler, the bronchodilator; salbutamol. This means that the imaging methods could also be valuable in clinical trials of new lung disease treatments.
This development has the potential to detect early declines in lung function and improve care for asthma, chronic obstructive pulmonary disease (COPD), and lung transplant recipients.
The team, comprising experts from Newcastle and Sheffield universities and NHS Trusts in both cities, published their findings in Radiology.
Use in lung transplants
A further study, published in JHLT Open and co-authored by Professor Andrew Fisher, Professor of Respiratory Transplant Medicine at Newcastle University, examined patients who had received a lung transplant for very severe lung disease.
Survival rates after a lung transplant vary. On average, 83 out of 100 patients are alive one year after a lung transplant, and 55 out of 100 are alive after five years. Chronic rejection, where the immune system attacks the donor lungs, is a common issue in lung transplant recipients.
The team scanned transplant recipients’ lungs and collected MRI pictures and precise measurements that showed how the air containing the gas reached different areas of the lung. Next, the team scanned those who either had normal lung function or who were experiencing chronic rejection after lung transplant.
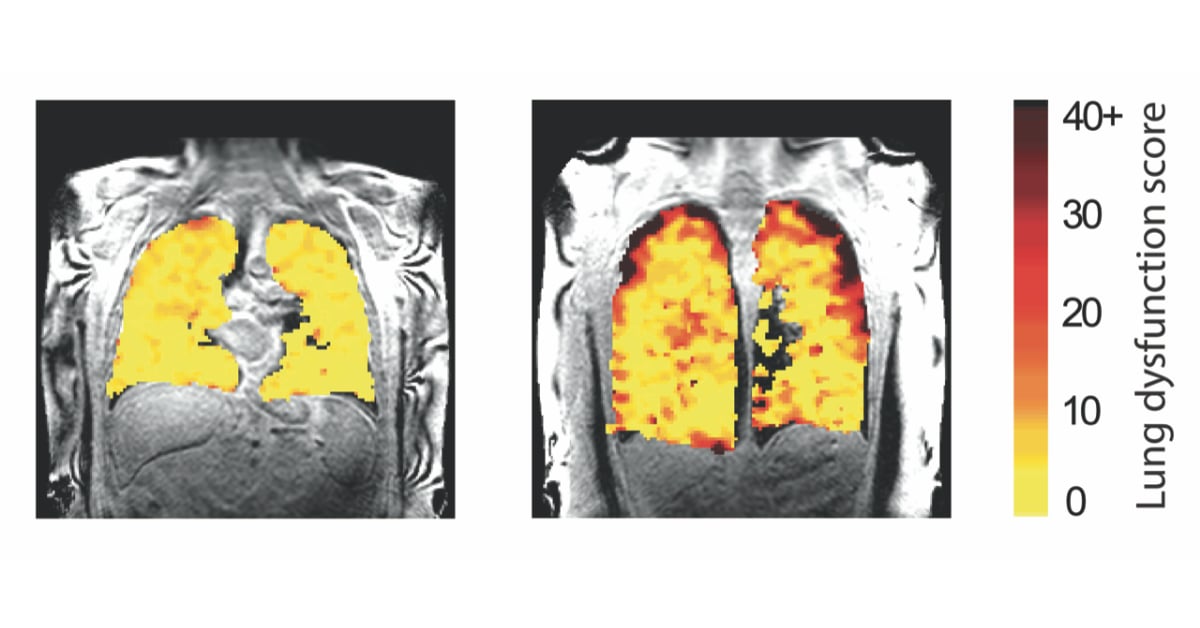
Lung function MRI showing measurements in lung transplant recipients.
In those with chronic rejection, the precise measurements showed poorer movement of air to the edges of the lungs, most likely due to damage in the very small breathing tubes (airways) in the lung. This is a feature typical of chronic lung transplant rejection, also known as chronic lung allograft dysfunction.
Better outcomes for patients
This new way of scanning the lungs has great potential for significantly improving the clinical management of lung transplant recipients and other lung diseases in the future.
'We hope this new type of scan might allow us to see changes in the transplant lungs earlier and before signs of damage are present in the usual blowing tests. This would allow any treatment to be started earlier and help protect the transplanted lungs from further damage.'
Professor Andrew Fisher
This new lung scan technology represents a new tool to better understand respiratory disease and to help develop new treatments. The team at Newcastle are currently working with colleagues in the NHS to assess how the scans can inform radiotherapy treatment for lung cancer by minimising the side effects of radiotherapy on a patient's lung function. These innovations are fuelled by physicists, bioscientists and clinicians working together to develop new technologies that address important questions of human health.
You might also like
- read the paper published in Radiology: Assessing Lung Ventilation and Bronchodilator Response in Asthma and Chronic Obstructive Pulmonary Disease with Fluorine 19 MRI. Pippard BJ, Neal MA, Holland CW, Maunder AM, Forrest I, Lawson RA, Fisher HF, Matthews JNS, Wild JM, Simpson AJ, Thelwall, PE. Radiology. DOI: https://doi.org/10.1148/radiol.240949 (n.b. live date 24th Dec)
- read the paper published in JHLT Open: Dynamic 19F-MRI of pulmonary ventilation in lung transplant recipients with and without chronic lung allograft dysfunction. Neal MA, Bos S, Holland CW, Hollingsworth KG, Meachery G, Nair A, Lordan JL, Fisher AJ, Thelwall, PE. JHLT Open. DOI: https://www.jhltopen.org/article/S2950-1334(24)00116-2/fulltext
- view the press release: New scan method unveils lung function secrets
- find out more about the academics involved in this study:
- Professor Peter Thelwall, Professor of Magnetic Resonance Physics, and Director of the Centre for In Vivo Imaging
- Professor Andrew Fisher, Professor of Respiratory Transplant Medicine at Newcastle Hospitals NHS Foundation Trust and Newcastle University
- explore the research and work done at the Centre for In Vivo Imaging
- find more statistics and information about lung disease at NHS England
